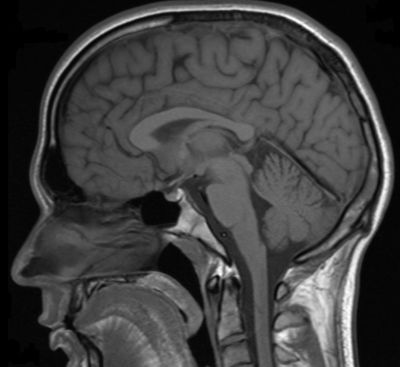
Mapping the complex interaction of brain, spinal cord, blood and cerebrospinal fluid (CSF) is required to unveil the dynamics of the brain in health and disease.
Normal pressure hydrocephalus (NPH) is a neurological condition caused by an accumulation of cerebrospinal fluid in the brain. The overlap of symptoms and findings with other neurodegenerative pathologies such as Alzheimer’s disease hampers diagnosis. The lack of understanding of the intra-cranial mechanics and the difficulty of acquiring detailed measurements within the brain add to treatment limitations.
To address the challenge of resolving disease mechanisms, the EU-funded DINUMA (Development of an integrated numerical model of the intra-cranial space (including the brain parenchyma, blood flow and cerebrospinal fluid) for clinical application) project proposed to develop a multi-scale numerical platform of the intra-cranial dynamics. In this context, researchers developed a novel bottom-up structural model for the brain parenchyma and a multiscale approach to the ventricular CSF flows. Investigations of the intra-cranial pressure dynamics in health and disease demonstrates how a better understanding of parenchymal ad CSF dynamics can improve clinical diagnostics.
The bottom-up structural model builds on tissue microstructure and micro-deformations to reconstruct the global interaction between the parenchyma and its environment. Despite underlying elastic cellular properties, time delays required for the extra-cellular fluid to re-equilibrate throughout the cellular matrix confer visco-elastic and strain-rate dependent properties to brain tissue, an observation that has been supported experimentally. More importantly, under constant load, the brain progressively deforms as fluid seeps out of the extra-cellular space, an observation that may have implication for the pathogenesis of NPH.
Multi-scale simulations of CSF dynamics demonstrated that although wall motion and choroid plexus pulsation affected CSF dynamics in the central regions of the ventricles, the near-wall dynamics and wall shear-stresses were dominated by the pulsations of the ependymal cilia. This demonstrated that intra-cranial dynamics are a result a complex responses at the cellular level.
Clinically, the CSF outflow resistance is used as a measure for intra-cranial dynamics in NPH patients. The procedure entails an infusion test, and calculation of CSF outflow resistance using an approximation that is not always satisfactory. Preliminary in vitro results demonstrated significant improvement in these calculations when accounting for the visco-elastic properties of the brain, as predicted with the DINUMA model. Accurate estimation of intra-cranial dynamics is therefore of high clinical relevance.