Anaemia, associated with chronic kidney disease, is a serious complication affecting millions of European patients. Using anticalin scaffolds, an EU-funded study aims to develop a novel therapy for tackling anaemia.
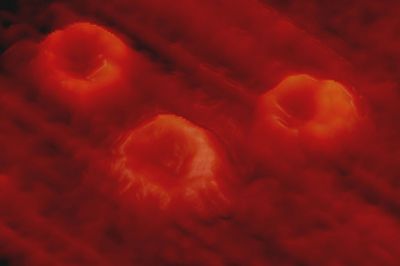
Functional iron-deficient anaemia is characterised by elevated blood
levels of hepcidin. Hepcidin is a peptide that regulates the entry of
iron into the circulation. Elevated hepcidin levels cause accumulation
of iron in the cells and reduced iron availability for red blood cell
production, or erythropoiesis.
A therapeutic approach of hepcidin inhibition will lead to increased erythropoiesis, normalising haemoglobin levels and reversing anaemia. The EU-funded project 'European consortium for anticalins as next generation high-affinity protein therapeutics' (
EUROCALIN) aims to develop and test this approach.
Partners from four EU countries already developed and will be clinically testing a novel therapeutic drug candidate antagonising hepcidin. The therapeutic drug candidate is a specific binder called Anticalin. It is a novel scaffold-derived protein from the lipocalin family of binding proteins.
Significant progress achieved during the first three years has brought the project to the point of the beginning of the clinical study. The proof-of-concept of reversing anaemia by inhibiting hepcidin was demonstrated in animals. Rat hepcidin-specific Anticalin reversed anaemia in animals in two weeks. The immunogenicity risk of the drug was found to be low.
A 28-day toxicity study established the safety of the drug. No undue tissue accumulation or adverse effects were observed, including for the group with the highest administered dose level. The team has established the manufacturing process for the drug and produced materials for the phase I study. The phase I clinical study of PRS-080-PEG30 in healthy volunteers was approved.
This project unifies the research efforts of European academia and industry in the field of new protein scaffolds. Anti-hepcidin therapies hold great promise to improve anaemia and patients' erythropoietic responses. They can reduce or eliminate the need for potentially toxic parenteral iron repletion, benefiting patients in Europe and internationally. Clinical validation of a unique, safe and effective therapeutic drug candidate is an area of high medical need.