In the EU, traumatic brain injuries (TBI) account for four times as many
years of life lost as diabetes, and they cause more lost working years
than cancer, stroke and HIV put together. Of the 1.6 million people who
suffer a TBI in the EU every year, 70,000 are in a life-threatening
situation and a further 100,000 will be left with a permanent
disability. Yet treating TBI patients can be particularly difficult due
to the complex nature of the brain, a lack of investment in R&D and
the individual nature of each injury.
The
TBICARE project – a joint initiative between eight partners in Finland (
VTT Technical Research Centre of Finland ,
GE Healthcare Finland ,
University of Turku ), France
Complexio , Lithuania
Kaunas University of Technology and the UK (
Imperial College London ,
University of Cambridge ,
GE Healthcare UK
) – is collecting data from hundreds of TBI patients and using it to
build a predictive model that will improve care. The system will allow
doctors to enter data from tests in the emergency department and will
predict the most effective course of treatment for each individual
patient. The project is part of a wider drive to use ICT to help
clinicians diagnose and treat more effectively using ICT tools that pool
existing but fragmented data and knowledge on the human body and can be
used to model outcomes – the concept of the
‘Virtual Physiological Human’ .
The project partners are hopeful that the predictions made by the
model will lead to more accurate diagnoses and better treatment. While
the prototype is still being validated, data from the recently-started
EU
Seventh Framework Programme
(FP7) CENTER-TBI project is expected to help optimise it. Equally,
several versions of the prototype are under evaluation by doctors at the
Turku University Central Hospital in Finland and the Addenbroke
Hospital in the UK, for research purposes only, with a view to have a
clinical tool in several years. Such tool will ease the day-to-day
clinical work of doctors and will revolutionise the ER-care and
treatment of traumatic brain injury.
According to
Dr Mark van Gils
, TBICARE’s scientific coordinator, ‘Improved diagnostics provided by
our system can have a potentially tremendous impact on TBI and its
aftermath. Costs related to TBI are not just the costs of care, but also
costs from loss of productive years, reduced quality of life, even
death – not forgetting the considerable impact on the family and friends
of the injured ones… An improvement of 1% would mean yearly savings of
EUR 1 billion in Europe alone.’
Increasing Knowledge – Improving Care
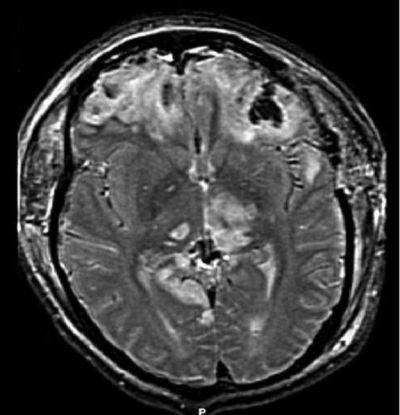
Dr Mark van Gils explains that under the project ‘patients are
tested for many different things when they arrive at an emergency
department. Their care team would look their awareness and reactivity,
and at how much oxygen is in their blood, for example. They also explore
the potential of more sophisticated measurements – for example testing
for proteins that indicate different types of damage to the patient's
brain tissue in their circulation, and using imaging to look for
internal bleeding. We want to see which tests give the best indicators
of the patient’s likely outcome.’
The TBICARE model will predict which injuries should be treated
first, and how they should treat them, as well as helping guide the care
team through the patient’s stabilisation and recovery.
The EU’s FP7 has provided EUR 3 million in backing over three years
to help build the tool. TBICARE project will end in August 2014.
Useful Links
A second chance for injured brains